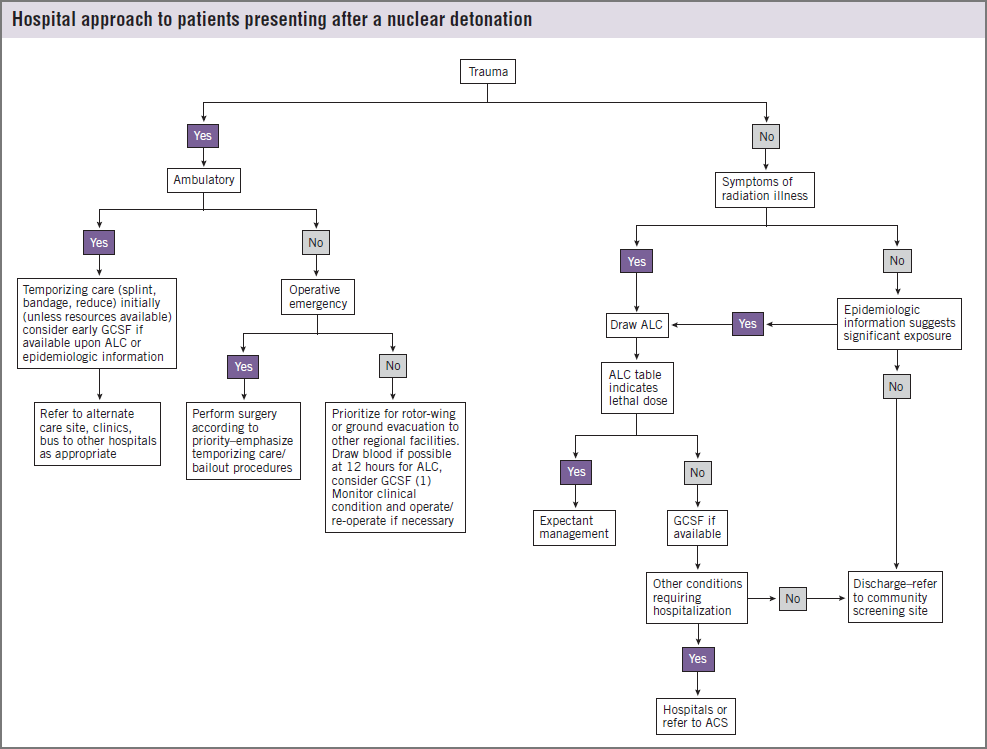
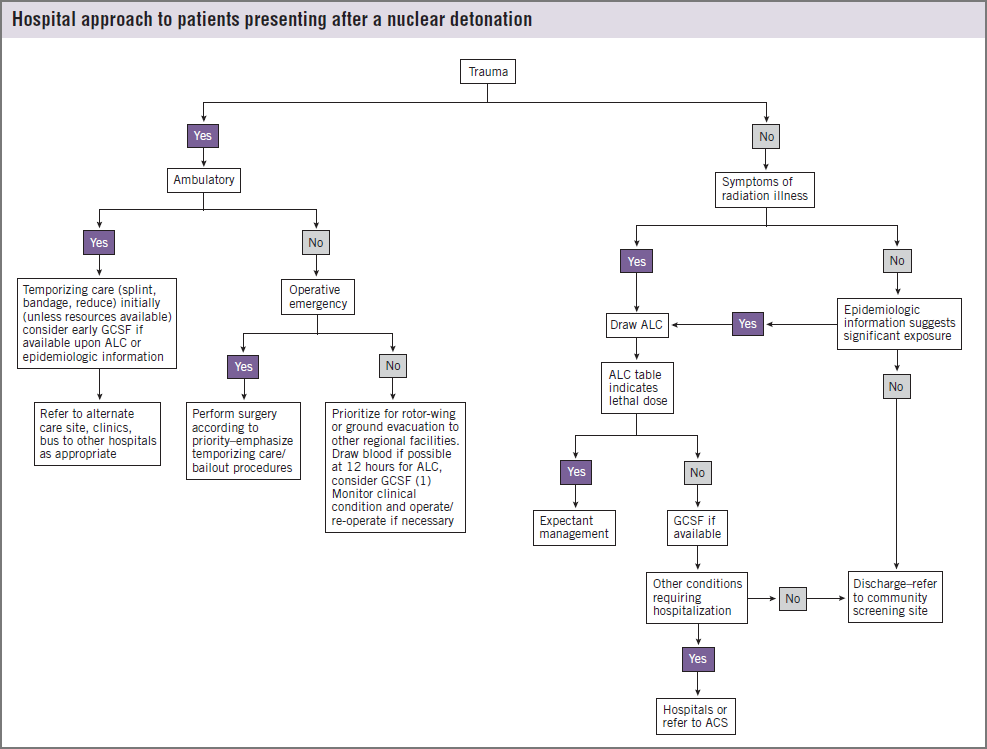
Hospital Approach to Patients Presenting after a Nuclear
Detonation
-
Source: Hick JL, Weinstock DM, Coleman CN, Hanfling D,
Cantrill S, Redlener I, Bader JL, Murrain-Hill P, Knebel AR.
Health Care System Planning and Response for a Nuclear
Detonation. Disaster Med Public Health Prep. 2011 Mar;5 Suppl
1:S73-88. See Figure 1 [PubMed Citation],
Full Text
(PDF - 197 KB)
-
This graphic and article are part of the
Scarce Resources Project, a series of 10 articles about medical care after an
IND when resources may be scarce and standards of care
may not be "normal".
-
This graphics assumes hospital resources are
inadequate for demand but
not overwhelmed. See
Resource Availability and Crisis Standards of Care
-
Abbreviations:
- ACL: absolute lymphocyte count
-
GCSF: granulocyte colony stimulating factor, a
myeloid cytokine
- ACS: alternate care site
-
Additional guidance
-
Attempt to estimate whole body radiation dose
-
Perform
targeted physical exam
looking for signs and symptoms of
Acute Radiation Syndrome
-
If resources available, augment clinical data with
biodosimetry lab data (single or serial CBCs and
differential)
-
Use
geographic dosimetry information
(Dose reconstruction)
-
As "physical radiation exposure information" becomes
available hours after the event, people may be
triaged to "not needing radiation assessment" if
they are not in radiation zones.
-
Understand that patients with
combined injury (significant
whole body radiation dose plus trauma/burns) have a
worse prognosis than patients with only one type of
injury.
-
Temporizing care for severely injured victims may be
palliative care only.
-
Consult senior incident managers in your facility
to understand whether
normal, contingency or crisis standards of care are
in place.
-
Re-evaluate radiation victims periodically, as
their status and resource availability status may change
over time.
-
See also: