Burn Triage and Treatment of Thermal Injuries in a Radiation Emergency
- Introduction
- Basics of burn injuries
- Emergency burn care
- Secondary survey and resuscitation
- Preventing, monitoring and treating early burn complications including compartment syndromes and inhalation injury
- Extended burn care to recovery: burn excision and reconstruction
- Supportive care and burn critical care
- Treatment of burns in austere, mass casualty conditions
- American Burn Association
Caveats:
- This page describes the diagnosis and treatment of skin injury due to thermal effects.
- For skin injury due to radiation effects, see REMM's Cutaneous Radiation Syndrome page.
- For burn issues in large mass casualty incidents with austere conditions, see “Treatment of Burns in Austere, Mass Casualty Conditions” section on this page.
Note:
- Content on this version of the REMM burn page was created in collaboration with the American Burn Association.
- The key consultants include: Drs. Joshua Carson, Rachel Williams, Colleen M. Ryan, William Hickerson, and James C. Jeng, with assistance from Annette Matherly, R.N.
- See entire List of REMM consultants which includes list of burn consultants from prior versions of REMM.
Introduction
- Following a radiation mass casualty emergency, especially a nuclear detonation, physical trauma with or without thermal burns (flash burns or flame burns) will be an immediate concern.
- An air burst type of nuclear detonation, will likely result in more burn victims than will a ground burst detonation of equal magnitude.
- Patients with combined injuries (radiation and trauma ± thermal burns) are known to have increased mortality compared to those who have a single type of injury.
- The increased mortality could be due many factors including the following
- Local and systemic radiation effects complicating other injuries
- Medical specialists in one area (e.g. burn, trauma or radiation injury) being less familiar with sophisticated, emergency diagnosis and treatment of other injury types.
- Conjoint multispecialty teams having little experience working together in large mass casualty incidents that involve radiation
- Temporary austere conditions, where the usual personnel, equipment, space, medications are not available
- Uncertainly about optimal ways to implement temporary “crisis standards of care” in a complex, austere environment
- The medical response to the thermal-injury aspect of radiological/nuclear mass casualty incidents will require immense resources to comprehensively manage patients’ burns.
- The management of seriously burned patients in the first few hours can significantly affect their long-term outcome.
- It is important that the patient be managed optimally in the early hours after injury to optimize the outcome.
- The complexity, intensity, multidisciplinary character and expense of the care required by an extensively burned patient have led to the development of specialty care burn centers.
- With the limited number of available and dedicated burn beds and burn specialists in any one region of the US, transfer of patients to specialized burn centers throughout the country will likely be needed.
- Consultation with an American Burn Association-verified burn center is recommended.
- Until patients can be transferred to burn centers (pre-existing or improvised) with a complete burn team, immediate care of the burned patients will require significant real-time guidance and training from burn experts remotely and/or via mobile burn core-medical teams.
- Consultation with an American Burn Association-verified burn center is recommended.
Basics of Burn Injuries
- Key concepts
- Thermal trauma and cutaneous radiation burns are complex disease processes with
- Direct tissue injury (e.g. skin and/or respiratory systems for thermal burns and cutaneous damage (but non-thermal injury) for radiation burns
- Pathologic systemic inflammatory response
- Multitude of potential secondary complications
- Systemic response to effects of burn injury and burn shock
- Systemic inflammatory response to burn injury
- Large burns generate a very intense systemic inflammatory response
- Massive burns generate one of the most intense inflammatory states seen in clinical medicine
- Burn Shock and Resuscitation
- Burn shock results principally from a combination of hypovolemic and vasodilatory shock.
- Treatment/avoidance of burn shock requires fluid resuscitation carefully titrated to maintain perfusion
- Inadequate volumes of fluid resuscitation will allow hypoperfusion, resulting in both secondary end organ damage as well as further expansion of the initial burn injury
- “Over-resuscitation” (administration of excessive volumes of fluids) can also cause serious injury and mortality via the life- and limb-threatening complications of edema
- Systemic inflammatory response to burn injury
- Thermal trauma and cutaneous radiation burns are complex disease processes with
- Burn depth: key descriptor and prognostic factor for burn injuries
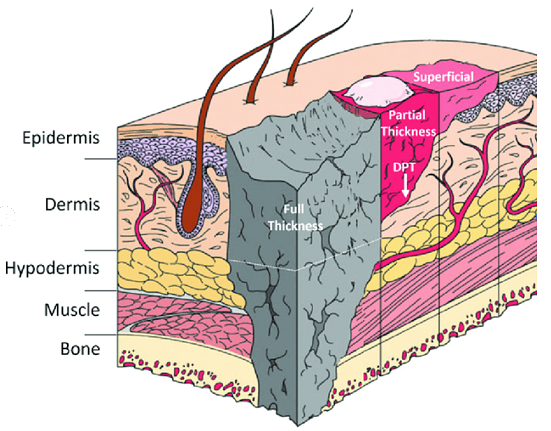
Source of graphic above: D’Arpa P, Leung KP, Toll-Like Receptor Signaling in burn Wound Healing and Scaring. Adv Wound Care (New Rochelle). 2017 Oct 1;6(10):330-343.
Note: The injury depths shown above are superficial, partial-thickness, deep partial-thickness (DPT), and full-thickness cutaneous burns which extend to hypodermis, shown by dotted line, or deeper than the dotted line.- Severity of burn injury is significantly correlated to the depth of injury
- Other key prognostic factors include total body surface area involved with burn, location of the injury (including pulmonary), age of the patient, and selected complicating, pre-existing systemic illnesses.
- Levels of burn injuries
- Superficial burns (aka first-degree burns)
- Dry, red, painful ("sunburn"), blanches.
- Akin to sunburn
- NOT counted in calculations of total burn surface area (TBSA)
- Partial Thickness Burns (Superficial Partial and Deep Partial thickness)
- The deeper the burn (aka second-degree), the slower the healing
- This outcome is thought to be related to fewer skin adnexa (appendages) for re-epithelialization
- Skin adnexa include: hair follicles, sebaceous glands, apocrine sweat glands, eccrine sweat glands
- Superficial Partial Thickness Burns
- Moist, red, blanching, blisters, extremely painful
- Deep Partial Thickness Burns
- Pale to white, drier, less blanching, less pain
- Takes up to 3 weeks or longer to heal via secondary intention.
- The deeper the burn (aka second-degree), the slower the healing
- Full Thickness Burns (aka third-degree)
- Destruction/death throughout the dermis
- Leathery texture, color varies, loss of sensation
- Superficial burns (aka first-degree burns)
- Severity of burn injury is significantly correlated to the depth of injury
- Inhalation Injury and Pulmonary Complications
- Airway deformity and compromise are potential severe complications
- Swelling to airway (vocal cords) either from local injury or as a component of the global body edema in large burns can eventually occlude airway
- Inhaled poisons may accompany burns
- Carbon monoxide (CO) poisoning
- Disables transport by binding to hemoglobin, resulting in anoxic injury
- Hydrogen cyanide poisoning
- Hydrogen cyanide is another product of incomplete combustion that may be inhaled in enclosed space fires. It occurs primarily from the combustion of synthetic products such as carpeting, plastics, upholstered furniture, vinyl
- and draperies. Hydrogen cyanide is a potent and rapid cellular poison.
- Carbon monoxide (CO) poisoning
- Smoke inhalation injury
- Smoke particles damage mucosal lining of proximal and distal airways.
- Sloughing mucosa collects in distal airway-- cast formation causes distal atelectasis or even bronchial obstruction (“mucosal plugging”)
- Note: pulmonary symptoms rarely grossly manifest within first 24hrs -- generally evolves over 48-72hrs
- Airway deformity and compromise are potential severe complications
- Secondary Injuries / Early Complications
- Extremity circulatory complications
- Limb Strangulation – “Eschar Syndrome”
- Circumferential (or near-circumferential) deep-partial- or full-thickness burns can create a functional tourniquet around the extremity as swelling limbs are cut off by noncompliant scar tissue
- Extremity compartment syndrome
- Extensive muscular swelling can overwhelm the limited volume capacity of extremity fascial compartments, leading to compromise of perfusion and ischemic injury
- Limb Strangulation – “Eschar Syndrome”
- Thoraco-abdominal restriction and cardiopulmonary compromise
- Burns involving large segments of the thorax can create restrictive respiratory failure
- Burns involving large segments of the abdomen, when coupled with aggressive fluid resuscitation, can create an abdominal compartment syndrome, cardiovascular collapse refractory to fluid resuscitation.
- In both cases, immediate relief is accomplished by releasing the tension through escharotomy—incision of scar that allows separation and functional expansion
- Extremity circulatory complications
- Prognosis and triage of burn injuries
- Significant prognostic indicators
- Increasing burn size (Prognosis worsens with increasing total body surface area affected by burn.)
- Age: mortality for any given burn size increases with age after childhood
- Concurrent non-thermal trauma
- Presence of Inhalation Injury
- Selected pre-existing chronic diseases
- CAUTION: Progressive injury and risk of progression
- Patients with injuries that appear to be larger than 5% TBSA should be monitored and reassessed for 8-to-24 hours before finalizing triage
- NOTE: Very little is known about the mechanisms by which radiation injury effects burn prognosis and vice versa. It is clear, however, that combined injury worsens prognosis.
- Significant prognostic indicators
Emergency Burn Care
- Rescue
- Before addressing the injuries present, first priority is to prevent any additional injuries.
- This means protecting bystanders, rescuers, and providers from injury, and halting ongoing trauma (burns, bleeding) in the patient.
- Rescuer and provider safety must be addressed before engaging the patient (for rescue or care)
- Fire-compromised structures may be at risk for collapse
- Prolonged exposure to smoke-filled confines can be harmful to enter without proper breathing equipment.
- Patients or their clothing may on flames or still hot enough to burn on contact.
- Rescue from ongoing injury
- Extinguish/smother flames, remove patient from path of fire, smoke or any mechanical threats. Put out any flames in patient.
- If any possibility for carbon-monoxide poisoning (burned and trapped in an enclosed space), apply supplemental oxygen to flush out CO.
- Cooling
- Small burns: may be cooled gently with cool water (recommend at least 20 min)
- Large burns: only actively cool tissue that is still at burning temperatures.
- Be aware of the risk of hypothermia from cooling.
- Before addressing the injuries present, first priority is to prevent any additional injuries.
- Primary Survey
- Once ongoing harm/injury has been arrested, the burned patient should be immediately assessed and stabilized from a mechanical trauma standpoint using principles of Advanced Trauma Life Support.
- The Primary survey includes
- Airway maintenance with cervical spine protection
- Breathing and ventilation
- Circulation and Cardiac Status with hemorrhage control
- Disability, Neurological Deficit and Gross Deformity
- Exposure (Completely undress the patient, examine for associated injuries and maintain a warm environment.)
- Danger of distraction
- Survivable thermal injuries do not represent a mortal threat within the first “golden” hour from injury.
- By far, the most likely cause of death within the first hour from injury is a missed/ignored traumatic injury
- Providers with limited burn experience must take care not to allow the novelty of the burn injury to distract them from adhering to the basic principles of trauma management
- Initiating Resuscitation with fluids
- In large burns, significant intravascular fluid loss begins shortly after injury.
- Initiating resuscitation as soon as possible helps minimize the ultimate severity of burn by maintaining perfusion to the viable portions of injured tissue.
- What to do
- Insert a large bore intravenous catheter (through unburned skin, if possible). Burns greater than 20% should have 2 large bore, indwelling venous catheters, especially during transport.
- In the pre-hospital and early hospital settings, prior to formally calculating the Total Body Surface Area (TBSA) burned, the initial fluid rates for patients with visibly large burns are based on a rough estimate of TBSA burned. [See below in secondary survey for fluid rate formula]
- Hourly fluid rates (termed “adjusted fluid rates”) should be adjusted to reflect updated TBSA estimate once formal assessment of burn surface area is perfomed in the Secondary Survey.
- Warming of the patient may be needed
- Measures should be taken to protect patients from hypothermia due to compromised skin protection.
- Hypothermia can drastically complicate burn shock, and it is far easier to prevent then it is to reverse
Secondary Survey and Resuscitation
- About the Secondary Survey
- The secondary survey does not begin until the primary survey is completed and after initial fluids are started.
- A secondary survey includes the following elements
- History (injury circumstances and medical history)
- Accurate pre-injury patient weight
- Complete head-to-toe evaluation of the patient
- Determination of percent Total Body Surface Area burned (see below)
- Apply adjusted fluid rates after TBSA determination (see below)
- Obtain indicated labs, X-rays and studies
- Monitor fluid resuscitation (see below)
- Pain and anxiety management
- Psychosocial support
- Determination of percent total body surface area (TBSA) burned
- In adults: "Rule of Nines" is used as a rough indicator of % TBSA; see table and diagram below.
Anatomic Surface
% of total body surface
Head and neck
9%
Anterior trunk
18%
Posterior trunk
18%
Arms, including hands
9% each
Legs, including feet
18% each
Genitalia
1%
- In children: use the Lund-Browder diagram below to modify the rule of nines and assign percent TBSA.
- Children have proportionally larger heads (up to 20%) and smaller legs (13% in infants) than adults
- Palmar hand surface of the child is approximately 1% TBSA
Lund-Browder diagram for estimating extent of burns in children (Print Lund-Browder diagram):
% Total Body Surface Area
(Adapted from The Treatment of Burns, edition 2, Artz CP and Moncrief JA, Philadelphia, WB Saunders Company, 1969) - In adults: "Rule of Nines" is used as a rough indicator of % TBSA; see table and diagram below.
- Adjusting, monitoring and titrating fluid resuscitation
- Once burn size (TBSA) has been formally estimated, initial fluid rate should be adjusted to reflect the size of injury.
- The adjusted fluid rates are calculated according to the table below.
Category Adjusted fluid rate
Age and weight
Adjusted fluid rate
Flame or scald
Adults and older children (≥14 years old)
2 ml LR x kg x % TBSA
Children (<14 years old)
3 ml LR x kg x % TBSA
Infants and young children (≤30kg)
3 ml LR x kg x % TBSA
PLUS D5LR at maintenance rate
Electrical injury
All ages
4 ml LR x kg x % TBSA - Monitoring response to fluids
- Check the patient’s urinary output and physiological response to decide further titration.
- Titrating fluid resuscitation
- It is better to increase fluids based on response than to attempt to remove excess fluids once given.
- Some patients including those with a delayed start of fluid resuscitation prior dehydration, or inhalation injuries may require more than the estimated fluids. Again, the adjustments to fluid rates are based on patient response.
- Wound Care
- During initial or emergent care, wound care is of secondary importance
- Advanced Burn Life Support recommendations from the American Burn Association
- Cover wound with clean, dry sheet or dressing: NO WET DRESSINGS
- Simple dressing if being transported to burn center (The burn care team will need to see the wound.)
- Sterile dressings are preferred but not necessary
- Covering wounds improves pain
- Cover wound with clean, dry sheet or dressing: NO WET DRESSINGS
- Elevate burned extremities above heart level when possible.
- This reduces edema, and thus increases perfusion to marginally viable skin while minimizing the risk of compressive ischemia or compartment syndrome
- Maintain patient's temperature (keep patient warm)
- This reduces edema, and thus increases perfusion to marginally viable skin while minimizing the risk of compressive ischemia or compartment syndrome
- Hypothermia is a constant threat in patients with medium to large burns
- See Prototype /Template for Hospital Orders for Adults and Children for selected options wound care and burn therapies which should be directed by experts in burn diagnosis and treatment.
Preventing, monitoring, and treating early burn complications including compartment syndromes and inhalation injury
- Re-assessment of airway
- Watch for emergence/progression of upper airway swelling.
- Failure to resuscitate
- Some patients will continue to manifest signs of poor perfusion or even hypotension.
- Importantly, any failure of resuscitation should prompt comprehensive consideration of missed/evolving injury or new complication including
- Reassessment of burn size for progression;
- Reviewing trauma workup and
- Reassessing for any missed mechanical-trauma injury
- Extremity complications
- Most effective measure in preventing or forestalling extremity complications is to limit swelling by
- Elevating extremity
- Avoiding excessive fluid administration
- Constricting eschars / Eschar Syndrome
- Most complications caused by constricting burn eschar develop several hours into resuscitation as progressive edema.
- Any circumferential or near-circumferential burn scars should be noted and followed with serial exam for progressive constriction.
- Involved limbs should be elevated.
- Any indication of ischemia from constriction (eschar syndrome) should prompt escharotomy serious consideration of escharotomy, resources permitting.
- Distal pulses are the last remaining sign of perfusion in eschar or compartment syndromes.
- Deferring intervention until distal pulses are lost can result in loss of limb
- Escharotomies may save limbs (
- Maintain high index of suspicion in completely circumferential burns
- Incisions are made laterally and medially splitting eschar along entire limb
- Should be limited to burn eschar and limited space above and below (2-4cm in each direction).
- No need to incise the entire length of an extremity for a burn scar that only involves a short segment
- Will likely require surgical hemostasis
- Compartment syndrome
- Compartment syndrome develop when compartment tissue swells beyond the volume capacity of the compartment fascia
- Eschar syndrome is a major predisposing factor
- Fasciotomies are definitive management
- Requires surgical expertise and awareness of anatomy
- Surgical hemostasis is required
- Most effective measure in preventing or forestalling extremity complications is to limit swelling by
- Trunk Compartment Syndromes
- Chest Compartment Syndrome
- Increased peak inspiratory pressure (PIP) due to circumferential trunk burns
- Escharotomies through mid-axillary line, horizontally across chest/abdominal junction
- Abdominal Compartment Syndrome
- Pressure in peritoneal cavity > 30 mmHg (measure via Foley catheter)
- Signs: increased PIP, decreased urine output despite massive fluids, hemodynamic instability, tight abdomen
- Treatment - decompression via escharotomy
- Chest Compartment Syndrome
- Inhalation injury
- Watch for late emergence of inhalation injury
- Typically takes 24-48hrs to manifest
- Patients show progressive decline in pulmonary function, with increasing requirements for support required to maintain adequate oxygenation and ventilation
- Prior to pulmonary manifestations, inhalation injury is typically manifest via fluid requirements beyond those anticipated for a given size of burn
- Watch for late emergence of inhalation injury
Extended burn care to recovery: Burn excision and reconstruction
- General principles
- While small burns or medium burns that are superficial throughout can often be managed on an outpatient basis, deep burns and large represent an ongoing risk for morbidity and mortality until open wounds have healed and/or reconstructed.
- This process can take anywhere from days to months, depending on the severity of burn and patient factors.
- While small burns or medium burns that are superficial throughout can often be managed on an outpatient basis, deep burns and large represent an ongoing risk for morbidity and mortality until open wounds have healed and/or reconstructed.
- Early excision and reconstruction are major drivers of recovery in burn patients.
- However, these operations are quite specialized and resource intensive.
- When at all possible, excision and reconstruction of any large burns should be performed at a tertiary center.
- Fortunately, the window for accomplishing early excision is flexible.
- As such, in any situation where transfer to a burn center can be accomplished within a matter of days, excision should be deferred until after transfer.
- Excision
- Once a patient has been stabilized and resuscitated, the cornerstone of modern burn care is to get “source control” of the inflammatory nidus by excising all burned tissue from the body.
- Early excision: cornerstone of modern burn care
- “Early excision” refers to the practice of surgically excising burn wounds down to healthy tissue.
- “Early” is invoked to distinguish this practice from the prior standard of care, which involved leaving the burned in place as they gradually demarcated and separated from the underlying viable tissue on their own.
- The precise timeline for early excision is subject to care context, patient factors and surgeon preference.
- Reconstruction
- All wounds excised through full thickness of skin will require reconstruction, generally via autologous skin graft.
- Many deep-partial thickness wounds benefit from grafting as well, as a means to expedite recovery and minimize scarring complications.
- As with excision, autologous skin grafting large surface areas is an extremely resource-intensive process that entails significant physiologic stress and blood loss.
Supportive Care and Burn Critical Care
- Massive thermal injuries create a massive inflammatory and metabolic stress that renders the burn patient increasingly vulnerable to infection and other complications until burn wounds are healed.
- Nutrition
- Between the energy required to heal large wounds and the metabolic dysfunction induced by the inflammatory response to thermal injury, patients with large thermal injuries live in a state of functional malnutrition.
- Aggressive nutritional support is essential to sustain the patient through the process of wound healing.
- Infection
- The compromised skin barriers, inflammatory dysregulation and malnutrition all predispose patients with massive thermal injuries to opportunistic infections.
- The inflammatory response to burn complicates this infectious risk, as early signs and symptoms of sepsis are difficult to distinguish from basic burn response.
- Rehabilitation
- Regaining maximal function requires specialized, intensive physical and occupational therapy.
- Pain control
- Thermal injuries and their treatments are often tremendously painful.
- Given the prolonged nature of burn care, sophisticated pain management strategies are required to achieve a reasonable modicum of pain control without creating crippling narcotic dependence.
- Psycho-social support
- The trauma of the initial injury and that associated with acute burn represent tremendous psychological stressors
- In many cases, the injury event is associated with additional losses such as injury to or loss of love ones, loss of home or possessions, or public catastrophe
- Social-psychiatric support systems and professional treatment during acute care and thereafter are often necessary to restore psychiatric and emotional function.
Treatment of Burns in Austere, Mass Casualty Conditions
- Standard burn treatment recommendations may need to be modified significantly in large incidents with temporary austere conditions, until normal capacity is restored.
- Several thoughtful, detailed monographs and papers review in detail key triage issues that are likely to arise during the various large, mass casualty incidents that REMM discusses, particularly an radiation emergency involving a nuclear detonation
- Military burn references
- Joint Trauma System Clinical Practice Guideline for Burn Care (PDF - 1.08 MB) (US Army, May 2016)
- Addresses burn injury assessment, resuscitation, wound care, and specific scenarios including chemical and electrical injuries.
- Reviews considerations for the definitive care of local national patients, including pediatric patients, who are unable to be evacuated from theater.
- Provides practical, evidence-based recommendations for optimal care of burn casualties in the deployed or austere setting
- Combat Casualty Care, Lessons Learned from OEF and OIG (Office of the Surgeon General, Department of the Army, USA, June 2011)
- Driscoll IR, Mann-Salinas EA, Boyer NL, Pamplin JC, Serio-Melvin ML, Salinas J, Borgman MA, Sheridan RL, Melvin JJ, Peterson WC, Graybill JC, Rizzo JA, King BT, Chung KK, Cancio LC, Renz EM, Stockinger ZT. Burn Casualty Care in the Deployed Setting. Mil Med. 2018 Sep 1;183(suppl_2):161-167. [PubMed Citation]
- Joint Trauma System Clinical Practice Guideline for Burn Care (PDF - 1.08 MB) (US Army, May 2016)
- Civilian burn references
- Kearns RD, Marcozzi DE, Barry N, Rubinson L, Hultman CS, Rich PB. Disaster Preparedness and Response for the Burn Mass Casualty Incident in the Twenty-first Century. Clin Plast Surg. 2017 Jul;44(3):441-449. [PubMed Citation]
- Peck M, Jeng J, Moghazy A. Burn Resuscitation in the Austere Environment. Crit Care Clin. 2016 Oct;32(4):561-5. [PubMed Citation]
- Jeng J, Gibran N, Peck M. Burn Care in Disaster and Other Austere Conditions. Surg Clin N Am 2014;94:893-907. [PubMed Citation]
- Kearns RD, Conlon KM, Valenta AL, Lord GC, Cairns CB, Holmes JH, Johnson DD, Matherly AF, Sawyer D, Skarote MB, Siler SM, Helminiak RC, Cairns BA. Disaster planning: the basics of creating a burn mass casualty disaster plan for a burn center. J Burn Care Res. 2014 Jan-Feb;35(1):e1-e13. [PubMed Citation]
- Kearns RD, Holmes JH 4th, Alson RL, Cairns BA. Disaster planning: the past, present, and future concepts and principles of managing a surge of burn injured patients for those involved in hospital facility planning and preparedness. J Burn Care Res. 2014 Jan-Feb;35(1):e33-42. [PubMed Citation]
- Conlon KM, Ruhren C, Johansen S, Dimler M, Frischman B, Gehringer E, Houng A, Marano M, Petrone SJ, Mansour EH. Developing and implementing a plan for large-scale burn disaster response in New Jersey. J Burn Care Res. 2014 Jan-Feb;35(1):e14-20. [PubMed Citation]
- “Acute Burn Procedures” have been recently reviewed
- Sheridan RL, Chang P. Acute burn procedures. Surg Clin North Am. 2014 Aug;94(4):755-64. [PubMed Citation]
- Military burn references
- Prognosis and triage
- Osler T, Glance LG, Hosmer DW. Simplified estimates of the probability of death after burn injuries: extending and updating the baux score. J Trauma. 2010 Mar;68(3):690-7. [PubMed Citation]
- Halgas B, Bay C, Foster K. A comparison of injury scoring systems in predicting burn mortality. Ann Burns Fire Disasters. 2018 Jun 30;31(2):89-93. [PubMed Citation]
- Ryan CM, Schoenfeld DA, Thorpe WP, Sheridan RL, Cassem EH, Tompkins RG. Objective estimates of the probability of death from burn injuries. N Engl J Med. 1998 Feb 5;338(6):362-6. [PubMed Citation]
- While “referral criteria” to a verified American Burn Center are established in the non-mass casualty setting, the recommendations are less clear in a large mass casualty setting
- Incident context
- In a small incident, any burn injury complicated by radiation injury would be recommended for transfer to a burn center.
- In a mass casualty incident, all referral decisions will require consideration of numbers of casualties, patient need, prognosis, system capacity, and available transportation.
- These decisions should all be made with input (in person or via remote consultation) from an experienced burn surgeon.
- Exporting experienced staff to unfamiliar sites may compromise efficiency.
- Preparedness planning references
- Kearns R, Holmes J, Cairns B. Burn disaster preparedness and the southern region of the United States. South Med J. 2013 Jan;106(1):69-73. [PubMed Citation]
- Kearns RD, Cairns BA, Hickerson WL, Holmes JH 4th. ABA Southern Region Burn disaster plan: the process of creating and experience with the ABA southern region burn disaster plan. J Burn Care Res. 2014 Jan-Feb;35(1):e43-8. [PubMed Citation]
American Burn Association
- General principles
- The American Burn Association (ABA) is an organization of burn caregivers who have set up a network of Verified Burn Centers to assist with management of burn disasters.
- All burn patients should initially be treated with the principles of Advanced Burn and/or Trauma Life Support
- The American Burn Association has expertise in training and response
- Verified Burn Centers provide advanced support for complex cases and are accredited by
- Verified Burn Centers participate in disaster planning and have set up a network for transporting burn patients throughout the country.
- To find the nearest Verified Burn Center near you,
- Contact the ABA Web site: www.ameriburn.org or
- Email: info@ameriburn.org or
- Call: 312-642-9260
- Gibran NS et al., Summary of the 2012 Burn Quality Consensus Conference. J Burn Care Res. 2013 Jul-Aug;34(4):361-85. 6 key topics are reviewed
- Overview of Quality Initiatives
- Psychological Outcomes
- Burn Resuscitation
- Nutrition Outcomes
- Functional Outcomes
- Burn Wound Healing Outcomes

