Use of Blood Products in a Radiation Emergency
- Summary of key information
- Principles of transfusion-associated graft-versus-host disease (TA-GVHD) prevention in radiation event emergencies
- Kinds of blood and blood components that should be irradiated
- Illustration of blood product irradiation
- Background information about transfusion issues and policies
- Graft vs. Host Disease (GVHD) Treatment
- Recipient risk factors associated with TA-GVHD
- Patient indications for blood irradiation
- Platelet transfusion guidance
- Red cell transfusions in children
- References
Note:
- This page does not provide official guidelines for use of blood or blood products.
- It is an aggregation of key peer-reviewed publications.
- Practitioners are encouraged to provide care as appropriate and feasible during a mass casualty radiation incident and consult experts in managing patients with radiation injury, e.g. Radiation Injury Treatment Network.
Summary of key information
- High-dose whole body radiation exposure induces hematopoietic cytopenias potentially requiring transfusion of blood products.
- Cytopenias requiring transfusion occur typically 2 to 4 weeks after high-dose radiation, although time to nadir varies by patient, dose from exposure, and dose rate. See illustration showing time-dose effects of radiation.
- Blood loss requiring transfusion may also result from trauma associated with the radiation incident and gastrointestinal losses from a variety of causes.
- Red blood cells, platelets, and whole blood that will be transfused to radiation victims should undergo the following procedures:
- 25 Gy of external radiation to prevent transfusion-associated graft-versus-host disease (TA-GVHD)
- Leukocyte reduction to diminish the risk of:
- Febrile non-hemolytic reactions
- Immunosuppressive effects of blood transfusions
- Platelet alloimmunization
- Cytomegalovirus infection
- In the setting of a mass casualty incident, if neither irradiation nor leukocyte reduction is available, lifesaving blood products should NOT be withheld.
- Recommendations vary among professional societies, countries, and facilities at what threshold blood product transfusion should be performed given a limited evidence base.
- During very large radiation incidents, available regional blood supplies may be constrained, at least initially, potentially making it difficult to transfuse using “standard” criteria.
- The table below provides IAEA's guidelines for transfusion of blood products for hematopoietic-ARS, in small incidents. In large incidents, constraints in the blood supply system, the number of victims, and individual patient risk factors may necessitate changes to standard transfusion protocols.
Criteria for Substitution Therapy for Hematopoietic Type Acute Radiation Syndrome
Patient's individual condition Threshold value Substitution therapy Close monitoring possible, no other complication, no bleeding Platelets: 10,000/μL Irradiated and leukoreduced
platelet concentratesClose monitoring not possible, increased risk of manifest bleeding Platelets: 20,000/μL Irradiated and leukoreduced
platelet concentratesAdditional trauma, survery, mass transfusion, cerebral edema Platelets: 50,000/μL Irradiated and leukoreduced
platelet concentratesAnemia Hemoglobin: 10 g/dL Irradiated and leukoreduced
packed red cellsSource: Medical Management of Radiation Injuries, IAEA Safety Reports Series No. 101 (IAEA, IFRC, PAHO, 2020, Table 13, page 42)
These recommendations are based on the METREPOL system (PDF - 580 KB) which addressed relatively small incidents.
- See additional references below.
Principles of transfusion-associated graft-versus-host disease (TA-GVHD) prevention in radiation event emergencies
- Avoid unnecessary transfusions.
- Avoid transfusions from first-degree relatives whenever possible because it increases the risk of TA-GVHD. If no other option is available, this blood must be irradiated.
- Transfusion of fresh blood, especially that stored for fewer than 3 days, should be avoided whenever possible, except for platelet concentrates.
- If allogeneic blood transfusion cannot be avoided, prevention of TA-GVHD by irradiation should be considered, especially for fresh blood.
- If blood transfusion is urgently required, and irradiated blood cannot be obtained immediately, there should be no hesitation about transfusing unirradiated blood or blood components.
- See references below.
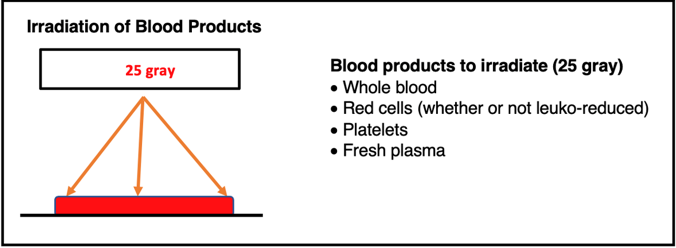
Kinds of blood and blood components that should be irradiated
- Whole blood
- Red blood cells, including leuko-reduced red blood cells and frozen red blood cells
- Platelets
- Note: See references below.
Illustration of blood product irradiation
Background information about transfusion issues and policies
- Transfusion-associated graft-versus-host disease (TA-GVHD) is a life-threatening consequence of transfusing blood into at-risk patients, including those with significant whole body radiation dose from exposure.
- If patients receiving large doses of whole-body radiation need blood products for any reason, TA-GVHD must be avoided, as treatment is difficult and rarely successful.
- In TA-GVHD, donor lymphocytes in transfused blood attack recipient organs and tissues. The donor cells recognize recipient HLA, proliferate via lymphoblastic transformation, and are not eliminated by host immune defenses.
- The fresher the blood, the higher the risk of TA-GVHD, especially with blood used within 3 days after donation.
- Typical TA-GVHD presents with fever, generalized erythema 1 or 2 weeks after transfusion, followed by liver dysfunction, diarrhea, and bone marrow failure with pancytopenia. Most patients die of multi-organ failure within 1 month of transfusion.
- TA-GVHD occurs at a higher rate in patients with no history of blood transfusions and in patients who receive blood from relatives.
- Leukocyte reduction by filtration is not sufficient to prevent PT-GVHD, but it is recommended because it diminishes the following:
- Febrile non-hemolytic reactions
- Immunosuppressive effects of blood transfusions
- Platelet alloimmunization
- Cytomegalovirus infection
- Blood and blood product irradiation will prevent TA-GVHD.
- Both irradiation and leukocyte reduction are recommended when these are available.
- See references below.
Recipient risk factors associated with transfusion-associated graft versus host disease
- Recipients with pre-existing immunodeficiency
- Congenital immunodeficiency
- Hematopoietic stem cell or organ transplantation
- Fetuses, low-birth-weight babies, and newborns
- Leukemia and malignant lymphomas
- Patients undergoing treatment with high doses of anticancer drugs, therapeutic radiation, or immunosuppression
- Recipients with NO pre-existing immunodeficiency
- Individuals from an HLA one-way matched donor (recipient lacks HLA antigens on donor cells)
- Patients undergoing surgery for cardiovascular disease and cancer operations
- Patients receiving accidental high doses of radiation
- Patients ≥ 65 years of age
Patient indications for blood irradiation
- Cytopenias from whole body radiation exposure
- Cardiovascular surgery
- Congenital immunodeficiency
- Hematopoietic transplantation
- Fetuses and low birth-weight infants
- Immunocompromised recipients of organ transplantation
- Recipient ≥ age 65 years
- Massive blood loss of severe trauma
- Malignant lymphomas, leukemias, hematological malignancies
- Solid tumor undergoing treatment with high-dose chemotherapy or radiation
- Note: Consult recent evidence-based disease-specific guidelines for more individualized recommendations.
Platelet transfusion guidance
- Bacterial Risk Control Strategies for Blood Collection Establishments and Transfusion Services to Enhance the Safety and Availability of Platelets for Transfusions: Guidance for Industry. (FDA, December 2020)
- Use of Platelet Transfusions, (Guidance from the British Society for Haematology, January 2022)
- Kaufman RM, Djulbefovic B, et al., Platelet Transfusion: A Clinical Practice Guideline from the AABB; An Intern Med 2015; 162(3):205-213.
- For adults
- Schiffer CA, Bohkle K, Delaney M et al, Platelet Transfusion for Patient with Cancer: ASCO Practice Guideline Update. J Clin Oncol. 2018 Jan 20;36(3):283-299. [PubMed Citation]
- For children
- Patel RM, Josephson C, Neonatal and pediatric platelet transfusions: current concepts and controversies. Curr Opin Hematol 2019;26(6):466-472. [PubMed Citation]
- Nellis ME, Goel R, Karam O, Transfusion Management in Pediatric Oncology Patients, Hematol Oncol Clin North Am 2019;33(5):903-913. [PubMed Citation]
- Nellis ME, et al., Executive Summary of Recommendations and Expert Consensus for Plasma and Platelet Transfusion Practice in Critically Ill Children: From the Transfusion and Anemia Expertise Initiative – Control/Avoidance of Bleeding (TAXI-CAB), Pediatr Crit Care Med 2022; 23(1):34-51. [PubMed Citation]
Red cell transfusions in children
Unlike adults, children RBC transfusion management is not totally dependent on hemoglobin level alone. See the references below for consensus recommendations from the Pediatric Critical Care Transfusion and Anemia Expertise Initiative (TAXI) for RBC transfusion practice in critically ill children. Note that these references almost exclusively at critically ill pediatric patients for reasons other than bone marrow suppression.
- Valentine SL, Bembea MM, Muszynski JA, Cholette JM, Doctor A, Spinella PC, Steiner ME, Tucci M, Hassan NE, Parker RI, Lacroix J, Argent A, Carson JL, Remy KE, Demaret P, Emeriaud G, Kneyber MCJ, Guzzetta N, Hall MW, Macrae D, Karam O, Russell RT, Stricker PA, Vogel AM, Tasker RC, Turgeon AF, Schwartz SM, Willems A, Josephson CD, Luban NLC, Lehmann LE, Stanworth SJ, Zantek ND, Bunchman TE, Cheifetz IM, Fortenberry JD, Delaney M, van de Watering L, Robinson KA, Malone S, Steffen KM, Bateman ST; Pediatric Critical Care Transfusion and Anemia Expertise Initiative (TAXI); Pediatric Critical Care Blood Research Network (BloodNet), and the Pediatric Acute Lung Injury and Sepsis Investigators (PALISI) Network. Consensus Recommendations for RBC Transfusion Practice in Critically Ill Children From the Pediatric Critical Care Transfusion and Anemia Expertise Initiative. Pediatr Crit Care Med. 2018 Sep;19(9):884-898. doi: 10.1097/PCC.0000000000001613. PMID: 30180125; PMCID: PMC6126913.
- Doctor A, Cholette JM, Remy KE, Argent A, Carson JL, Valentine SL, Bateman ST, Lacroix J; Pediatric Critical Care Transfusion and Anemia Expertise Initiative (TAXI); Pediatric Critical Care Blood Research Network (BloodNet), and the Pediatric Acute Lung Injury and Sepsis Investigators (PALISI) Network. Recommendations on RBC Transfusion in General Critically Ill Children Based on Hemoglobin and/or Physiologic Thresholds From the Pediatric Critical Care Transfusion and Anemia Expertise Initiative. Pediatr Crit Care Med. 2018 Sep;19(9S Suppl 1):S98-S113. doi: 10.1097/PCC.0000000000001590. PMID: 30161064; PMCID: PMC6125789.
- Spinella PC, Tucci M, Fergusson DA, et al. Effect of Fresh vs Standard-issue Red Blood Cell Transfusions on Multiple Organ Dysfunction Syndrome in Critically Ill Pediatric Patients: A Randomized Clinical Trial. JAMA. 2019 Dec 10;322(22):2179-2190. [PubMed Citation]
References
Ensuring the US blood supply
- Adequacy of the National Blood Supply, Report to Congress 2020 (HHS) (PDF - 5.34 MB), includes discussion of ensuring the adequacy of the blood supply in the case of public health emergencies in Chapter 4. (HHS)
General references about transfusion guidelines
- Mueller MM, Van Remoortel H, Meybohm P, Aranko K, Aubron C, Burger R, Carson JL, Cichutek K, De Buck E, Devine D, Fergusson D, Folléa G, French C, Frey KP, Gammon R, Levy JH, Murphy MF, Ozier Y, Pavenski K, So-Osman C, Tiberghien P, Volmink J, Waters JH, Wood EM, Seifried E; ICC PBM Frankfurt 2018 Group. Patient Blood Management: Recommendations From the 2018 Frankfurt Consensus Conference. JAMA. 2019 Mar 12;321(10):983-997. [PubMed Citation]
- Editorial on this key paper: Zeller MP, Kaufman RM. Safeguarding the Patient's Own Blood Supply. JAMA. 2019 Mar 12;321(10):943-945. [PubMed Citation]
- AABB has made publicly available as a pdf document the Circular of Information for the Use of Human Blood and Blood Components(AABB, American Red Cross, America's Blood Centers, Armed Services Blood Program, revised June 2024)
- A Compendium of Transfusion Practice Guidelines, Edition 4.0 (American Red Cross).
- BCSH Blood Transfusion Task Force. Guidelines on gamma irradiation of blood components for the prevention of transfusion-associated graft-versus-host disease. Transfus Med. 1996 Sep;6(3):261-71. [PubMed Citation]
- Asai T et al. Guidelines for irradiation of blood and blood components to prevent post-transfusion graft-vs.-host disease in Japan. Transfus Med. 2000 Dec;10(4):315-20. [PubMed Citation]
- Kaufman RM, Djulbegovic B, Gernsheimer T, Kleinman S, Tinmouth AT, Capocelli KE, Cipolle MD, Cohn CS, Fung MK, Grossman BJ, Mintz PD, Sesok-Pizzini DA, Shander A, Stack GE, Webert KE, Weinstein R, Welch BG, Whitman GJ, Wong EC, Tobian AA. Platelet Transfusion: A Clinical Practice Guideline From the AABB. Ann Intern Med. 2014 Nov 11. [PubMed Citation]
- Schiffer CA, Bohlke K, Delaney M, Hume H, Magdalinski AJ, McCullough JJ, Omel JL, Rainey JM, Rebulla P, Rowley SD, Troner MB, Anderson KC. Platelet Transfusion for Patients With Cancer: American Society of Clinical Oncology Clinical Practice Guideline Update. J Clin Oncol. 2018 Jan 20;36(3):283-299. doi: 10.1200/JCO.2017.76.1734. Epub 2017 Nov 28. PMID: 29182495.
- Deschner M, Vasanthamohan L, Zayed S, Lazo-Langner A, Palma D, D'Souza D, Omar Gilani S, Gabriel Boldt R, Solh Z. The impact of red blood cell transfusion on mortality and treatment efficacy in patients treated with radiation: A systematic review. Clin Transl Radiat Oncol. 2021 Dec 16;33:23-29. doi: 10.1016/j.ctro.2021.12.002. PMID: 35243018; PMCID: PMC8885402
Graft versus host issues and blood irradiation
- Kopolovic I, Ostro J, Tsubota H, Lin Y, Cserti-Gazdewich CM, Messner HA, Keir AK, DenHollander N, Dzik WS, Callum J. A systematic review of transfusion-associated graft-versus-host disease. 2015 Jul 16;126(3):406-14. doi: 10.1182/blood-2015-01-620872. Epub 2015 Apr 30. PMID: 25931584
- Zeiser R, Blazar BR. Pathophysiology of Chronic Graft-versus-Host Disease and Therapeutic Targets. N Engl J Med. 2017 Dec 28;377(26):2565-2579. [PubMed Citation]
- Del Lama LS, de Goes EG, Petchevist PC, Moretto EL, Borges JC, Covas DT, de Almeida A. Prevention of transfusion-associated graft-versus-host disease by irradiation: technical aspect of a new ferrous sulphate dosimetric system. PLoS One. 2013 Jun 7;8(6):6-9. (Note: This reference is included because it has an excellent literature review of GVH. Readers should not infer an endorsement of a specific irradiator product or technique.) [PubMed Citation]
- BCSH Blood Transfusion Task Force. Guidelines on gamma irradiation of blood components for the prevention of transfusion-associated graft-versus-host disease. Transfus Med. 1996 Sep;6(3):261-71. [PubMed Citation]
- Theusinger OM, Stein P, Spahn DR. Transfusion strategy in multiple trauma patients. Curr Opin Crit Care. 2014 Dec;20(6):646-55. [PubMed Citation]
- Anderson K. Broadening the spectrum of patient groups at risk for transfusion-associated GVHD: implications for universal irradiation of cellular blood components. Transfusion. 2003 Dec;43(12):1652-4. [PubMed Citation]
- Webb IJ, Anderson KC. Transfusion-associated graft-verus-host disease. In: Popovsky MA, editor. Transfusion Reactions. Bethesda, MD: AABB Press, 2001: 171-186
- Asai T et al. Guidelines for irradiation of blood and blood components to prevent post-transfusion graft-vs.-host disease in Japan. Transfus Med. 2000 Dec;10(4):315-20. [PubMed Citation]
- Anderson KC, Goodnough LT, Sayers M, Pisciotto PT, Kurtz SR, Lane TA, Anderson CS, Silberstein LE. Variation in blood component irradiation practice: implications for prevention of transfusion-associated graft-versus-host disease. Blood. 1991 May 15;77(10):2096-102. [PubMed Citation]
- Leitman SF, Holland PV. Irradiation of blood products. Indications and guidelines. Transfusion. 1985 Jul-Aug;25(4):293-303. [PubMed Citation]
Platelet transfusion
- See REMM Bibliography about Platelet Transfusion
Transfusion of red cells
- Ortega R, Canelli RJ, Quillen K, Mustafa W, Kotova F. VIDEOS IN CLINICAL MEDICINE. Transfusion of Red Cells. N Engl J Med. 2016 Mar 17;374(11):e12. (See video associated with this article.) (This is a short basic review, not specifically related to radiation issues.) [PubMed Citation]

